|
Up to $70 Million to Be Awarded to Advance Alzheimer’s Disease Clinical Trials
At the close of 2017, the National Institutes of Health (NIH) is expected to award up to $70 million over five years to three physician-scientists to launch the Alzheimer’s Clinical Trials Consortium (ACTC), which will create a network of 35 Alzheimer’s disease trial sites across the country with the goal of finding new ways to treat or prevent Alzheimer’s. Dr. Reisa A. Sperling, director of the Center for Alzheimer Research and Treatment at Brigham and Women’s Hospital, and who serves as the principal investigator of the ACTC at both BWH and Massachusetts General Hospital and is also professor of Neurology at Harvard Medical School, will collaborate with colleagues at the Mayo Clinic and the Keck School of Medicine at the University of Southern California (USC) to accelerate clinical trials for Alzheimer’s disease and related dementia. In a press release from the hospital, Sperling is quoted as saying, “We must overhaul our current recruitment strategies for clinical trials, particularly to improve the diversity of our study participants and to reach people who do not yet have symptoms of Alzheimer’s disease…the new ACTC presents a terrific opportunity to innovate in recruitment, cognitive assessments, and neuroimaging for the next generation of Alzheimer’s trials.” The ACTC will also help researchers engage in new collaborations to test promising therapies and prevention strategies. Researchers at Brigham and their colleagues are leading efforts to find ways to intervene as early as possible before the first signs and symptoms of Alzheimer’s appear when some treatments are expected to be most effective. The objective of the ACTC is to offer the infrastructure, shared resources, and expertise to help surmount the hurdles in prevention, diagnosis, and treatment of the disease. Is Anxiety an Early Indicator of Alzheimer’s Disease? This is a question that we may be close to answering in the future. Investigators at Brigham and Women’s Hospital have examined the association of brain amyloid beta and longitudinal measures of depression and depressive symptoms in cognitively normal, older adults. Their findings, published in January by The American Journal of Psychiatry, indicate that higher levels of amyloid beta may be associated with increased symptoms of anxiety in certain individuals. These results support the theory that neuropsychiatric symptoms could be an early indicator of AD. According to first author Dr. Nancy Donovan, a geriatric psychiatrist at the hospital, “Rather than just looking at depression as a total score, we looked at specific symptoms such as anxiety. When compared to other symptoms of depression such as sadness or loss of interest, anxiety symptoms increased over time in those with higher amyloid beta levels in the brain. [The finding] suggests that anxiety symptoms could be a manifestation of Alzheimer’s disease before the onset of cognitive impairment. If further research substantiates anxiety as an early indicator, it would be important for not only identifying people early on with the disease but also, treating it and potentially slowing or preventing the disease process early on,” she explains. As anxiety is common in older people, rising anxiety symptoms may prove to be most useful as a risk marker in older adults with other genetic, biological, or clinical indicators of high AD risk. Donovan notes further longitudinal follow-up is necessary to determine whether escalating depressive symptoms give rise to clinical depression and dementia stages of Alzheimer’s disease over time.
0 Comments
Leave a Reply. |
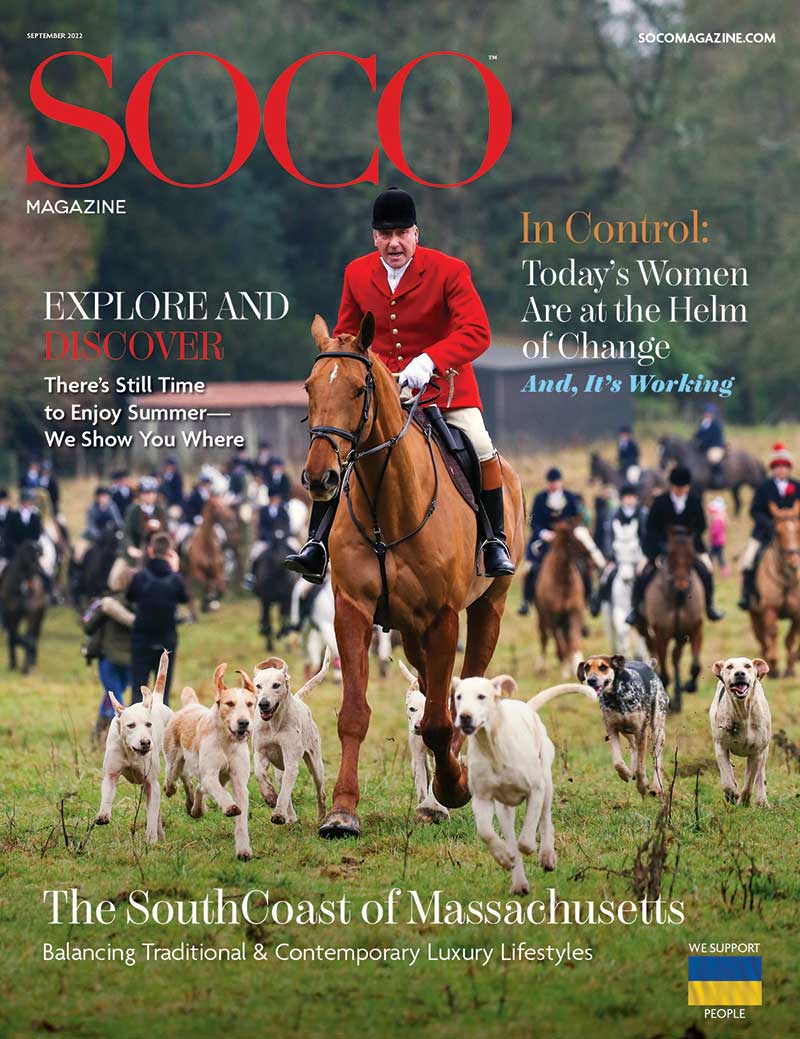
Click the cover above to receive a free digital subscription
Archives
June 2022
Categories
|